A photo oxidative collagen cross linking technique case study by Dr. Shaher Saad Eddin , OD, Amman-Jordan, Ophthalmology section contribution University Yerevan Armenia.
Developed to counteract the progressive corneal thinning and thus the progression of keratoconus. With cross linking an additional covalent binding between collagen molecules can be achieved, which stabilizes the collagen scaffold and changes several tissue properties.
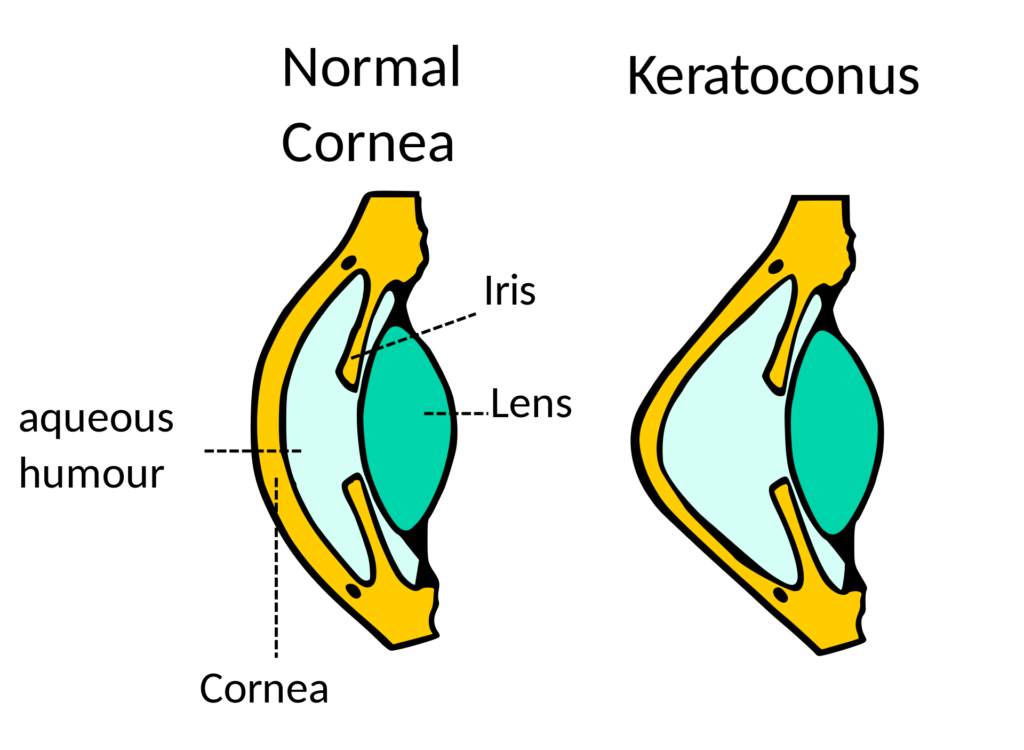
This is a measure to increase the rigidity of the cornea (in particular the stroma layer) to reduce the progression of keratoconus.
With the use of ultraviolet-A waves and after saturating the cornea layer with a vitamin B2 (Riboflavin) treatment.
Within a decade this has become a very successful treatment for keratoconus cases especially in early and moderate stages.
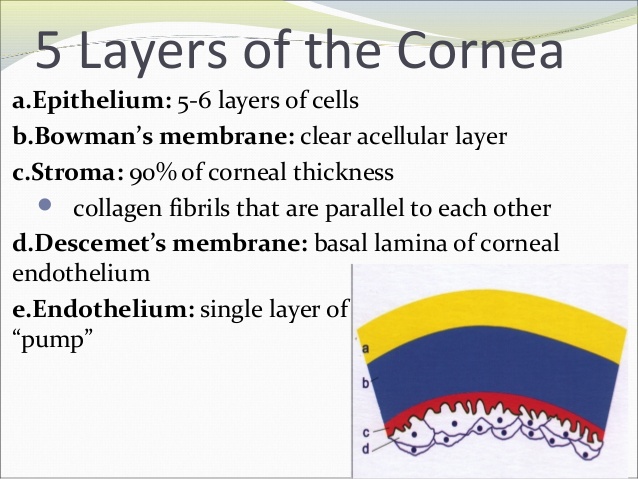
The Microanatomy of the human cornea
The human cornea has five layers. From the anterior (this is the outer cornea surface one can touch) to the posterior, the layers of the human cornea are:
This treatment started in Jordan in 2008 at the Eye Specialty Hospital
The goal of this treatment is to increase the rigidity of the cornea (stroma layer) by using ultra-violet-A waves after saturating the cornea’s stroma layer by vitamin B2 (Riboflavin) application.

Riboflavin (vitamin B2) has two essential functions. It absorbs UV irradiation and acts as a photosensitizer for the generation of a reactive oxygen species (singlet oxygen). In combination with UV light riboflavin forms radicals that cause the cross linking. When riboflavin penetrates the stroma sufficiently, it also shields the deeper tissues such as the eye lens, glass body (corpus vitreum) and the retina.

Although this process is relatively recent, but it has evolved over the past few years attracting more attention to determine patients which are eligible and a good success outlook.
These developments include the different techniques as well the UV-A devices to apply during the treatment.
There are three main surgical techniques:
- Epithelium off: which means removing the thin epithelium layer, the first layer, covering the cornea of the eyes’ surface. This allows for a faster penetration of the riboflavin.
- Epithelium on: Transepithelial corneal cross linking where the epithelium is remaining on the cornea’s surface. The corneal epithelial surface is remaining intact, which requires a longer riboflavin loading time to reach the stroma layer.
- Corneal pocket: this new technique is using a femtosecond laser technology to create a pocket inside the stromal layer and then inject the riboflavin inside the pocket.

There are diverse types of vitamin B2 which are useful when applying for the corneal cross-linking procedure.
- Riboflavin Dextran Isotonic Solution to penetrate the corneal stroma.
- Hypotonic 0.5% riboflavin solution without dextran.
According to the thickness of corneal as our experience has shown we use a hypotonic dextran free riboflavin for a cornea thickness less than 400μm and the isotonic dextran with a cornea more than 400μm.

Epithelium-off CXL
The miosis of the pupil is induced by the application of two drops of Pilocarpine before starting the treatment.
At the beginning the surgeon removes the epithelium layer of the cornea and instills a drop of isotonic riboflavin solution with dextran onto the cornea every 5 minutes for half an hour. What follows is to expose the cornea to the UV-A light for an additional half an hour and keeps instilling riboflavin onto the cornea.
After that the surgeon applies a bandage contact lenses onto the cornea for 4 or 5 days until the epithelial layer has grown again over the stroma layer of the cornea.
New device developments allow to reduce the time of irradiation treatment to expose the cornea for five minutes with UV-A light only.
Epithelium-on CXL
As mentioned beforehand the epithelium is remaining on the cornea.
Hypotonic riboflavin 0.5% solution without dextran is instilled to increase the permeability of the corneal epithelium and to increase the riboflavin penetration into the stroma and to achieve a higher UV-A light absorption.
This technique is recommended for patients with a cornea thickness less than 400μm (measured at the thinnest point of the cornea) and in patients older than 26 years with a slow progressive keratoconus. Not for pediatric patients 18 years or younger or those patients older than 26 years with a cornea thickness more than 400μm measured at the thinnest point.
Executive Summary
As by our experience the treatment epithelium-off cross linking is more effective than epithelium-on cross linking. But this kind of treatment a corneal thickness of more than 400μm should be present, otherwise we use the epithelium-on technique.
Although there are some advantages of the epithelium-on (trans-epithelial CXL) technique. A reduced risk of infection, corneal haze and delays in epithelial healing. Also, it allows for a quicker visual recovery and has less discomfort.
The latest technology development by creating a pocket inside the stroma layer using a femtosecond laser and inject the riboflavin into this pocket offers some procedural aspects such as reducing the surgeon treatment time and the patient’s discomfort.
Which patients might benefit most of it by the corneal cross linking techniques CXL?
Not all keratoconus patients will have a successful treatment via these techniques. The selection process is a very diligent task for the doctors offering such measures.
The highest success rates derive from patients with keratoconus at an early stage, such as I or II, and patients with ectasia post Lasik refractive surgery before suffering a significant drop of vision.
The goal of this treatment is to stabilize the progression changes of the corneal curvature, in conjunction to improve the patient’s visual acuity and the ability to wear glasses or contact lenses.
In some cases, we do cross linking pre-refractive surgery in very early stages of the keratoconus such as frost cone with a good corneal thickness and a small refractive error.
The treatment of a corneal ulcers is another case where we can use a corneal cross linking.
As mentioned before, the best results of this treatment are coming via a thorough patient selection process where the doctor is considering all the existing data and pre-measurements.
The doctor should do a routine exam of the eye, a visual acuity and refractive error test and a corneal topography.
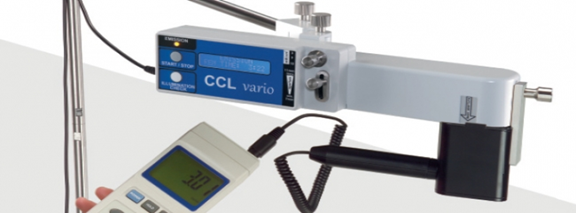
The development of UV-A light devices
The treatment by outdated devices of UV-A light was around 30 minutes for each eye, now there are devices allowing to reduce the irradiation time for just 5 minutes for each eye.
VEGA is sample of the first generation device.

CCL VARIO is the sample of the recent technology
We are looking forward to your questions.
The Optik Inspektor Team