Pathogenic role of Demodex mites in blepharitis
The optics inspector (Optik Inspektor) team believes that the following article by Jingbo Liu, Hosam Sheha, and Scheffer CG Tsenga is one of the most competent summary of eyelid inflammation (blepharitis). (Originally in English).
Abstract – Purpose of review in this study
A summary of the most important literature and our research experience on the Demodex infestation as a possible cause of eye infections, with a special focus on the Demodex Blepharitis (inflammation of the eyelids).
Recent findings on the Demodex blepharitis issue
The mite Demodex folliculorum ( English , German ) can cause anterior blepharitis (inflammation of the eyelid), which is associated with disorders of the eyelashes. The mite Demodex brevis can cause posterior blepharitis (conjunctivitis) with meibomian gland dysfunction (malfunction) and kerato-conjunctivitis (inflammation of the cornea). Tea tree oil treatments with either 50% eyelid abrasion or 5% eyelid massage are effective in fighting mites and reducing eye inflammation.
Introduction to Demodex mites and eye infections
Demodex mites are the most common microscopic ectoparasites on human skin. The rate of Demodex infection increases with age, being observed in 84% of the population over the age of 60 and in 100% of the population over the age of 70. In addition to the higher density in patients with rosacea, Demodex mites have also been observed as the cause of other skin diseases such as pityriasis folliculorum, perioral (oral rose) dermatitis, rash-like skin changes, facial pigmentation, bald scalp rash and even basal cell carcinoma. Since the eye is surrounded by raised parts of the body such as the nose, eyebrow and cheek, the eyelid is not as accessible to daily cleaning hygiene as the face. As soon as a demodex infection has established on the face, it can spread in the eyelids and lead to blepharitis. Nevertheless, the clinical significance of the Demodex infestation remains partially controversial, since it can also be found in asymptomatic patients. Therefore, Demodex blepharitis is often overlooked in the differential diagnosis of corneal and external diseases and no therapeutic options are considered. Here we will summarize the key literature and our research experience on the pathogenic potential of Demodex mites in the development of eye infections, with a special focus on the inflammation of the eyelids (blepharitis). Therefore, Demodex blepharitis is often overlooked in the differential diagnosis of corneal and external diseases and no therapeutic options are considered. Here we will summarize the key literature and our research experience on the pathogenic potential of Demodex mites in the development of eye infections, with a special focus on the inflammation of the eyelids (blepharitis). Therefore, Demodex blepharitis is often overlooked in the differential diagnosis of corneal and external diseases and no therapeutic options are considered. Here we will summarize the key literature and our research experience on the pathogenic potential of Demodex mites in the development of eye infections, with a special focus on the inflammation of the eyelids (blepharitis).

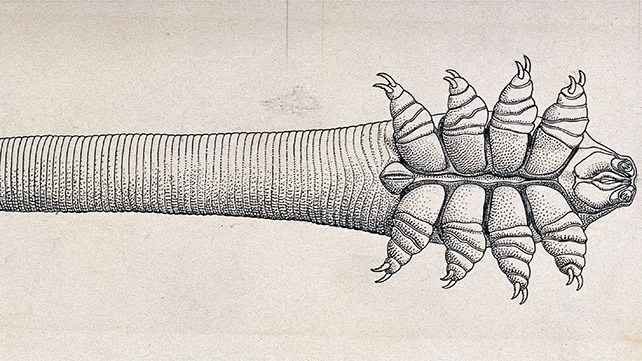
The life of the Demodex mite and humans
Two different types have been identified in humans: the Demodex folliculorum and Demodex brevis. In the eyelids, the D. folliculorum is located in the eyelash follicle (hair follicle), whereas D. brevis penetrates deep into the sebaceous glands and the Meibomian glands and searches for sebum, which is their most important source of nutrition. It can also be assumed that the mites feed on follicular and glandular epithelial cells (skin cells), which leads to direct damage to the edge of the lid. The life cycle of the Demodex mite from egg to larval stage is approximately 14–18 days, followed by 5 days in adulthood. Female animals can live an additional 5 days after laying their eggs. Due to the limited life span of adult mites, mating plays an important role in the reproduction of the Demodex infestation. In addition, the life of Demodex outside the living body is limited, so direct contact is required for mite transmission. It is therefore important to prevent mite mating and to avoid direct transmission as an indispensable treatment strategy.
Risk factors of Demodex blepharitis
Recently, we have a close correlation (interaction) between the severity of rosacea (acne rosacea called (German: Rotfinnen), copper rose or (German: Kupferakne), English) and the Demodex blepharitis. Rosacea predisposes patients to blepharitis mainly through the blockage of all oil-producing glands, which are necessary for a healthy epidermis (epidermis), and thus creates an environment on the skin that simplifies the infection. Other factors that promote mite spread include skin type photo-sensitivity, plenty of sunlight, alcohol consumption, smoking, stress, hot drinks, hot foods, and abrupt changes in temperature. Patients whose local or systemic immune status is impaired by external or systemic use of steroids or other immunosuppressive agents, or by diseases such as leukemia and HIV, are more likely to develop demodex mites.
Pathogenesis
Demodex blepharitis can be anatomically divided into anterior ( front ) and posterior (rear) blepharitis. The former relates to the infestation of eyelashes and follicles (hair follicles) by D. folliculorum, which accumulates at the root of the eyelashes, while the latter relates to the infestation of D. brevis in the meibomian gland. The following mechanisms of action are proposed to explain the pathogenic role of Demodex in blepharitis.
Direct damage
Demodex mites, especially folliculorum, consume epithelial cells on the hair follicle, which leads to follicle expansion, which can contribute to the formation of loose or incorrectly directed eyelashes. Micro-abrasion caused by mite claws can cause epithelial hyperplasia (excessive cell formation, German , English) and reactive hyperkeratinization (horny cell formation) around the base of the eyelashes and form cylindrical scales. D. brevis can block the openings of the meibomian glands, which leads to a malfunction of the meibomian gland with lipid tear deficiency (poor tear film quality). D. Brevis usually drills deep into the meibomian glands, and his chitinous exoskeleton is a foreign body that causes granulomatous (nodular, forming) reactions. Brevis was observed in the center of meibomian granulates, surrounded by epithelial cells, histocytes fibroblasts , lymphocytes and plasma cells. Thus, a potential cause of recurring and intractable (refractory) chalazia (chalacion). The hordeoleum (Hordeolum) is inflammation of the sebum in the edge of the eyelid and corner of the eye.
Vector for bacterial pathogens
Demodex mites can cause blepharitis by carrying bacteria on their surface, including streptococci and staphylococci. Super-antigens produced by these bacteria are also involved in the induction of rosacea. In addition, a bacterium in Demodex mites was found to be important in triggering an immune response from the host. Bacillus oleronius, which has recently been detected in Demodex mites, can stimulate the proliferation (proliferation, proliferation) of peripheral blood in the mono-nuclear cells in patients with rosacea. In our joint and prospective study, a strong correlation was also found between the positive serum immune reactivity towards the 83 kDa and 62 kDa Bacillus proteins, ocular demodex, facial rosacea and blepharitis.
Hypersensitivity reaction in the skin
The protein within the Demodex mite, as mentioned above, and its remnants or waste thereof, can trigger an inflammatory response by the host by delayed hypersensitivity or an immune response that has existed since birth. By examining 92 cases of papulopustular rosacea and in succession with 92 control subjects, consistent in age and gender, Georgala et al. (and colleagues) found that hair follicle involvement was accompanied by predominantly (90–95%) CD4 helper or inducer T cells with intensive perifollicular infiltrates. An increased number of macrophages and Langerhans cells was only observed in subjects with a positive D. folliculum.

Clinical manifestation (signs)
The main symptoms are itching, burning, foreign body sensation, crusting and reddening of the eyelid margin and blurred vision. Symptoms include cylindrical dandruff, loss of eyelashes, inflammation of the eyelid rim, meibomian gland dysfunction (dysfunction), blepharo conjunctivitis (inflammation of the conjunctiva at the edge of the lid) and Blepharo keratitis (inflammation of the cornea).
Skin and subcutaneous tissue disorders
In addition to the cylindrical scales found in Demodex blepharitis, persistent infestation of the eyelash follicles can lead to malalignment, ingrowth (trichiasis) or loss of eyelashes. Trichiasis can lead to trauma to the corneal epithelium, which leads to selective epithelial erosions („scratching“ of the cornea), followed by corneal ulcers and pannus formation in severe, long-standing cases.
Inflammation of the conjunctiva
Without proper hygiene, inflammation of the eyelid margin can spread to the conjunctiva, leading to a condition called blepharo-conjunctivitis. This misdiagnosed demodex-related conjunctivitis is usually resistant to conventional medication.
Our clinical experience shows that successful treatment of ocular demodicosis (hair follicle mite infestation in the eye) in adults eliminates Blepharo conjunctivitis when traditional therapies fail. Although Demodex has been identified as the cause of Blepharo conjunctivitis in adults, its role in children remains unclear. We recently reported 12 healthy pediatric patients with recurrent Blepharo conjunctivitis and demodex mite infestation. All patients showed a striking conjunctivitis, which was demonstrated by reddening with bulbi (eyeball) conjunctiva (conjunctiva) and papillary follicle reaction (nodule formation) of the tarsal conjunctiva (conjunctiva of the eyelids). All patients who „scrubbed“ or massaged the eyelid edges, to eradicate the mites showed a dramatic decrease in eye irritation and inflammation, and a decrease in the number of mites. These results suggest that Demodex is also an overlooked cause of apparently untreatable conjunctivitis in children
Demodex influences on the cornea
Inflammation from the edge of the eyelid, especially the meibomian glands, can also spread to the cornea, depending on the severity. Demodex infestation can cause various corneal lesions and other corneal diseases. Corneal vascularization (ingrowth of blood vessels into the superficial cornea), marginal infiltration (inclusions), superficial opacity and nodular (raised) scar. Interestingly, D. brevis is more commonly associated with such a corneal manifestation, although the likelihood of D. brevis, which normally occurs only in the sebum and meibomian glands, is quite rare in epilated eyelashes. Future studies are needed to determine whether such an unusually high infection rate of D.
diagnosis
The potential criteria for the diagnosis of Demodex blepharitis:
1. Clinical observation and high suspicion index in conjunctivitis, corneal inflammation, in adult patients or conjunctivitis and frequently recurring stye (chalazion) in young patients who do not heal against conventional treatments. Abnormalities in the event of eyelash failure or uneven growth.
2. Slit lamp examination: typical cylindrical scales at the root of the eyelashes.
3. Microscopic confirmation: detection and counting of Demodex eggs, larvae and adult mites in epilated eyelashes.
Treatment
Various demodex mite treatments have been used. 1% mercury oxide ointment, pilocarpine gel, sulfur ointment and camphor-containing oil. Most of them apply an ointment on the base of the eyelashes at night to trap mites as they emerge from their burrow and / or move from one eyelash / follicle to the next. However, on an in vitro microscopic observation over a period of 150 minutes, we found that D. folliculorum is resistant to a variety of common antiseptic solutions in adults, including 75% alcohol and 10% povidone iodine, as well as such antimicrobial substances such as Erythromycin and metronidazole can, however, be killed by tea tree oil (TTO) depending on the dose. In contrast to baby shampoo, TTO lid peeling not only removes cylindrical scales from the eyelash root, but also stimulates embedded mites to migrate from the follicle (hair follicle) to the surface of the skin. The 50% solution TO directly kills the mites, while the lid massage with a 5% break the life cycle in such a way that mating is prevented. Aside from the Demodex eradication, TTO treatments dramatically relieved symptoms and significantly alleviated and healed the inflammation around the eyelid margin, conjunctiva and cornea. Since TTO can also have antibacterial, fungicidal (fungus) and anti-inflammatory effects, we cannot attribute its therapeutic benefits in the treatment of the above-mentioned eye diseases solely to the effects of mite killing. Since the Demodex also serves as a vector of the skin organisms, the comorbidity (co-disease), which is based on a symbiotic relationship of the bacterium oleronius in Demodex mites, also justifies the consideration of a therapeutic strategy to kill the symbiotic bacterium via oral antibiotics such as tetracycline. Daily eyelid peeling with 50% TTO and eyelid massage with 5% TTO ointment can effectively fight the Demodex infestation in the eye in vivo. This is shown by the fact that the demodex value was reduced to zero within 4 weeks in a majority of the patients. which is based on a symbiotic relationship of the bacterium oleronius in Demodex mites, also the consideration of a therapeutic strategy to kill the symbiotic bacterium via oral antibiotics such as tetracycline. Daily eyelid peeling with 50% TTO and eyelid massage with 5% TTO ointment can effectively fight the Demodex infestation in the eye in vivo. This is shown by the fact that the demodex value was reduced to zero within 4 weeks in a majority of the patients. which is based on a symbiotic relationship between the bacterium oleronius in Demodex mites, and the consideration of a therapeutic strategy to kill the symbiotic bacterium via oral antibiotics such as tetracycline. Daily eyelid peeling with 50% TTO and eyelid massage with 5% TTO ointment can effectively fight the Demodex infestation in the eye in vivo. This is shown by the fact that the demodex value was reduced to zero within 4 weeks in a majority of the patients.
Summary
Demodex blepharitis is a frequently overlooked external eye disease. The pathogenesis (cause of the disease) of Demodex blepharitis when eye inflammation was triggered was further clarified. The modified method for taking and counting eyelashes facilitates and improves the diagnosis of Demodex infestation. Tea tree oil shows promising potential for the treatment of Demodex blepharitis by reducing the number of Demodex with additional antibacterial, antifungal and anti-inflammatory effects.
Conclusion
Demodex mites play an important role in the appearance of a number of diseases of the eye surface, such as Demodex blepharitis, malfunction of the meibomian gland, conjunctivitis and corneal lesions. The eye infestation is closely related to the systemic infestation. Further studies are needed to develop simple and sensitive diagnostic methods as well as more effective and specific treatment regimens.
Statement from the Optik Inspektor / optics inspector team
It should be noted that the inflammation of the eyelid in particular, and the inflammation of the anterior segment in general, are diagnosed far too little in Germany under the aspect of the named Demodex mites. This type of mite is from the hair follicle family. This is probably due to a lack of knowledge of the following studies and scientific facts. There are only a few specialists in Germany who deal with this in practice on patients. There is hardly a German-language article on the Internet that treats the eyelid inflammation in connection with the Demodex mite. These are mostly kept superficial, and often give false advice on cleaning the eyelashes and eyelid margins.
In contrast, a rare and good example of the topic on the Internet is that of the OSCB Berlin .
Consulting and support on this article: Dr. Joserine Samson, Gulf Eye Center Link , LinkedIn , ISCLS